The 10-Step Medical Billing Process

Medical billing involves submitting and tracking claims with payers to receive payment for medical services. It includes translating medical procedures and diagnoses into medical codes, preparing and submitting claims, and resolving any issues or denials to ensure timely reimbursement. In a hospital setting, medical coders and billers may work in various departments such as emergency medicine, radiology, and surgery. They may also be responsible for coding and billing for inpatient and outpatient services, as well as managing insurance claims and denials. Despite the importance of medical coding and billing, there are several challenges that medical coders and billers face.
How to Know Whether Your RCM Is Performing Well

The Certified Professional Biller (CPB) certification prepares medical billers with the technical knowledge and skills to maintain all aspects of the revenue cycle. Without deep knowledge and expertise in medical billing and the unique understanding of insurance requirements, provider reimbursement may be denied, delayed, or incomplete. Preauthorization is the process of obtaining approval from an insurance company before a service is provided to ensure coverage. It helps in reducing denied claims and is a critical step in the Medical Billing Process steps. Common denial codes include CO-50 (services not deemed medically necessary), CO-29 (the time limit for filing has expired), and CO-109 (claim/service not covered by this payer/contractor). Understanding these codes helps in the appeal process in medical billing and how to improve medical billing process.
How Virtual Medical Scribe Services Reduce Burnout and Improve Productivity
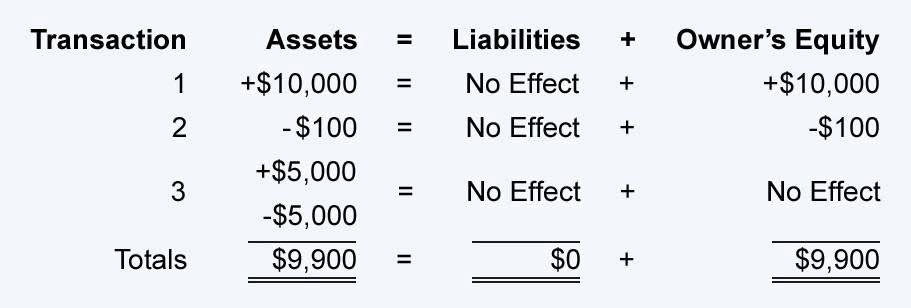
RCM helps strengthen revenue by minimizing claim denials, reducing days in accounts receivable, and increasing collections. As a result, healthcare providers receive correct and timely payments and optimize financial performance. Effective RCM also can help healthcare organizations comply with regulatory requirements and improve patient satisfaction. Revenue cycle management (RCM) is the process healthcare organizations use https://www.bookstime.com/ to manage financial operations related to billing and collecting revenue for medical services. RCM begins when a patient schedules an appointment and ends when the account balance is resolved through reconciliation of insurance payments, contractual adjustments, write offs, or patient payments. Denial management is an aspect of medical billing dealing with investigating, analyzing, correcting, and preventing claim denials.
- It involves ten critical steps to ensure that medical practices receive timely and accurate payments.
- This encoded information can be understood by all insurance companies and medical providers, and is used to generate bills and track payments.
- Diagnosis codes are key to describing a patient’s condition or injury, as well as social determinants of health and other patient characteristics.
- Here we’ll explore the basics of medical billing, review the steps included in most medical billing processes, and parse the differences between the related tasks of medical coding and medical billing.
- Although medical services are standardized through codes, the fees aren’t standardized.
- When a patient goes to a healthcare provider for a complete check-up, a superbill is made.
The importance of medical coding and billing in healthcare
Continuous monitoring and managing discrepancies are essential for a smooth adjudication process in medical billing. The Coordination of Benefits (COB) process determines the order in which multiple insurance plans will pay a claim. This is essential for avoiding duplicate payments and ensuring proper charge entry in the billing process. Contact us today to schedule a no-obligation demonstration of our industry-leading billing expertise. With over 12 years of experience, we excel in operational excellence, helping healthcare providers navigate the complexities of the medical billing landscape. In instances where patients have outstanding bills, Neolytix’s system identifies such cases and streamlines the process of engaging with collection agencies.
This is a digital/electronic network that Alberta Health uses for all these claims. Each of your interactions with your patient needs to be recorded — either in voice form, video, or written down. Every single procedure, every single encounter you have with that individual must be recorded for insurance purposes. You’ll need to present factual, irrefutable proof of everything you did and how you treated them. If your claim submission results in a nonzero balance for a patient who doesn’t have secondary insurance, you must send the patient a statement detailing their charges. You should also send an explanation of benefits detailing what the patient does and doesn’t get with their insurance plan.
Train for your career in medical billing and coding
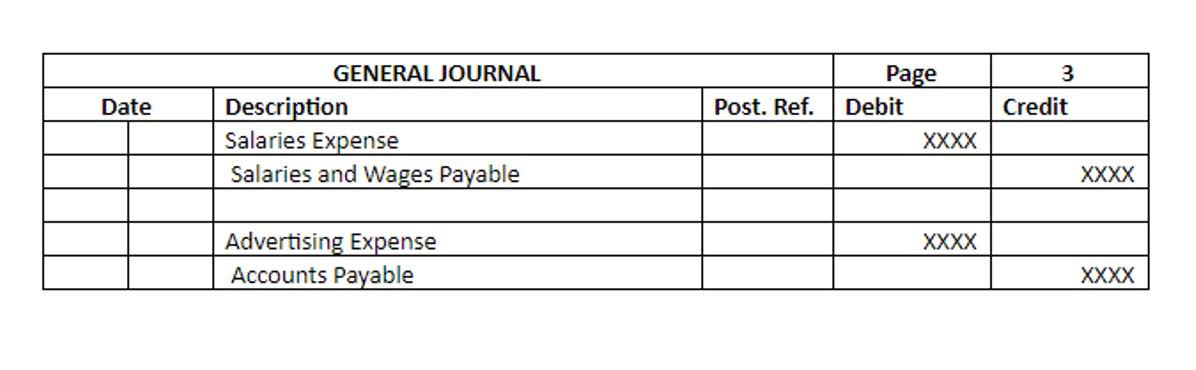
Good billing practices starts with the initial patient call, and sets the stage for full reimbursement. Coding, Billing and Transmitting primary & secondary claims to thousands of government payers and insurance companies, as well as Denial Management are all incredibly important to eliminating rejected claims. Once the claim has been processed, the patient is billed for any outstanding charges.
- In addition to their day-to-day responsibilities, medical billing specialists also typically work on special projects, such as developing new billing procedures or implementing new coding systems.
- It will include provider and clinician information, the patient’s demographic information and medical history, information on the procedures and services performed, and the applicable diagnosis and procedure codes.
- Medical coding is a process through which standardized codes are applied to the information contained in medical documents including physician’s notes, laboratory and other diagnostic results, and hospital records.
- But much more happens before, after, and between in the medical biller’s workday.
- While certain aspects of medical billing and coding overlap, they’re not identical tasks.
Types of Medical Codes
In a single day, medical billers and coders—particularly those who perform both functions—might need to decipher medical jargon, clarify a dispute with an insurance company and answer a patient’s billing questions. Medical coding and billing specialists play a key role in the healthcare industry. They are responsible for ensuring that healthcare providers receive proper reimbursement for their services, as well as for maintaining accurate patient records. These professionals must be familiar with a wide range of medical codes and billing procedures, and they must also stay up-to-date with changes in the healthcare industry. Medical billing, on the other hand, is the process of submitting claims to insurance companies and other payers to receive payment for medical services provided. Medical billing specialists are responsible for ensuring that claims are submitted accurately and in a timely manner, so that healthcare providers can receive payment for their services.
